Murray PHN

Murray PHN commissioned APMHA to deliver mental health services in line with the Stepped Mental Health Model of Care since 2018. The program continues to grow and expand across our funded catchments:
- Goulburn Valley Regions: Greater Shepparton, Strathbogie, Murrindindi and Mitchell Shires
- North East Regions: Albury/Wodonga, Alpine, Wangaratta, Benalla, Mansfield and Indigo Shires

Centralised Intake APMHA
APMHA has 2 dedicated FTE who provide central intake, triage, waitlist support, secondary consultation and program allocation to 37 clinicians.
Our workforce
Are a mix of employed and sub-contracted experienced clinicians who provide face to face, phone or video mental health counselling and support.
The workforce consists of: Psychologists, Mental Health Social Workers, Credentialed Mental Health Nurses, and Mental Health Occupational Therapists.
The programs:
Mild-Moderate care stream Psychological Therapy Services (PTS)
PTS provides free short term face-to-face or telehealth psychological services to eligible clients who have been identified as under-serviced and/or hard to reach. This includes support for those impacted by natural disasters such as drought, flood or bushfire.
This service targets;
PTS specialist streams include:
- Children’s Mental Health (o-13 yo)
- General Services (14yo+)
- Older Persons (65yo+) in residential aged care facilities
- Suicide Prevention Services (low risk intensive support)
Moderate-complex care stream Primary Mental Health Clinical Care Coordination (PMHCCC)
PMHCCC provides free therapeutic interventions and coordination of clinical services for eligible clients with severe and persistent mental illness.
This service targets;
Older Minds Mental Health Program for RACFs
The Older Minds Mental Health Program is a regional outreach service to RACFs in Goulburn Valley and North East. APMHA provides Psychological Therapy Services (PTS) to support the mental health needs of people living in RACFs. This service allows residents of registered RACFs to access similar mental health services available to those in the community. This service also provides mental health training and secondary consultation for aged care facility staff to enable timely identification of psychological distress in residents and appropriate referral.
Workforce Comments
I would like to provide some feedback regarding my experiences working as a contractor for this organisation. I joined the APMHA HealthCare team in early 2022 and feel privileged to work for such a professional, caring, and supportive team that immediately made me feel welcome and part of their community. During my time working for APMHA HealthCare, it is evident that the team provides exemplary health service and outcomes, ensuring access to quality care for all those who seek support. APMHA HealthCare is an excellent place to work with a great team spirit and a positive environment where I feel respected and, although small, my contributions are appreciated. I enjoy the professional yet friendly interpersonal relationships with team members, particularly Trish, Monique, Donal, and Tung.
– Dr Jane
APMHA is one of the best companies to work with as a contractor. I feel completely supported and included. I work with a great bunch of people and know that they have both the clients and my interests at heart.
– Liane Margis
Other Client Feedback:
- Genuine. All the assistance was relevant and when put into practice worked.
- Having sessions able to be done over the phone with all the COVID – 19 restrictions in place and that my feelings are validated I can feel that I can share or talk about my issues without judgement.
- How my provider listens and allowed us to both work together to create a solution.
- It was a very positive and growth changing experience for me. I no longer worry and I look for solutions and I love myself for the first time in my life and although sometimes it was very difficult to deal with situations I found dealing with them set me free.
- Feeling like some weight is lifted off my shoulders, I can finally make it through another day
- Everything, I have never experienced understanding compassion and support from another service that I have from this service I can never thank my clinician enough for helping me achieve the obstacles I have..
RACF Comments
RACF Staff:
- This service has been a welcome relief as the time spent with residents cannot always be given by staff. Residents feel ‘safe’ and the clinician can shed light into some issues that help us manage or increase care appropriately i.e Loneliness, medication advice, anxiety. Thank you so much
- The COVID period and multiple lockdowns have been hard for many residents, unable to have family/friends visit and the uncertainty of what is happening ‘in the outside world’. Having the Older Minds program was a great outlet for our residents to talk to. The residents look forward to their visit and staff have noticed a positive change in many
RACF Residents:
- I have never talked to anyone before about my problems, but I have found it very helpful
- Recently lost my husband of over 60 years. It has been helpful and comforting to have someone to talk to when staff are too busy

APMHA RACF Workforce:
The last 12 months working in the Aged Care space has been quite a challenge on many levels due to Covid lockdowns. There were times we were not able to go into the facilities due to the lockdowns and when we did enter lots of procedures were in place to protect the residents; including having to wear full PPE, completing risk assessments and completing covid tests were all part of the process.
The residents were hugely impacted psychologically by the lockdowns, unable to see family or friends; and on a few occasions they were confined to their rooms for lengthy periods of time. Sessions during these times focused around residents’ isolation and loneliness and the need to find meaningful activities to fill their long and lonely days. Often communication during the sessions proved even more challenging due to having to wear full PPE. Residents would often request” take that stupid bloody thing off!!!” Groups , outings and activities on the unit were unavailable during this time, some residents really struggled with the lack of routine and structure and not being able to leave the unit with family as they had done previously.
During this time only “essential” services were able to enter the unit, this meant that external providers such as the hairdresser or volunteers were unable to come in as they had previously. Staff working on the units were frequently anxious, stressed, and short staffed. Often they were required to work longer shifts and perform duties they wouldn’t normally such as serving meals and working in the kitchen. Often staff would want a chat, reassurance and support from someone outside the unit.
Despite all the challenges over the past 12 months I have found the work challenging and rewarding and feel privileged to have been able to work with such a resilient client group and an amazing group of healthcare workers. Thank you.
– Kerry Coyle
HeadToHealth Shepparton & Seymour

In early 2022, HeadtoHelp services across Victoria rebranded to the new name HeadToHealth and in March 2022, we celebrated our first birthday of the HeadToHealth (H2H) program.
HeadToHealth sites have also been established in all other States through PHNs.
HeadToHealth is a free mental health and wellbeing service for people who may be experiencing psychological distress or who may need support.
How HeadToHealth works:
When you call HeadToHealth on 1800 595 212, an experienced mental health professional will conduct an initial assessment and work with you to find the best ways to get the help you need. Depending on the assistance you need, HeadToHealth may connect you with online support or an existing mental health service or a local HeadToHealth hub.
HeadToHealth staff provide various presentations to organisations about the programs and services. In September 2021, we co-presented with GoTafe for R U OK? Day to over 100 students who linked in via Zoom. APMHA donated two ipad mini’s for students.
12 months in review…
Over the last 12 months APMHA has continued to deliver this service in Seymour and Shepparton:


Comments:
“The clinician ‘heard me’ – it was the first time someone actually understood my story and helped me find a way through.”
- My counsellor understood me, helped & guided me.
- I had related to past experiences that were affecting my mental health so I could have some closure.
- My counsellor is practical, helpful and understanding. It made a huge difference to my state of mind & progressive improvement in head health.
- The quality of the individual
- My counsellor is so lovely and helpful . I always feel so much better after l have spoken to her.
- I found my counsellor so easy to talk to and very helpful. A lovely lady and she has given me some excellent strategies to work on.
“Care and professionalism shown to me”
- My counsellor is absolutely brilliant. The best help I have received ever.
- My counsellor is very knowledgeable about what she is telling me and makes me feel comfortable with her.
Effective. - No waiting time to start.
- Very competent
- My counsellor was always willing to listen and was very supportive of all the situations that arose
My counsellor would always keep in touch check in always easy to contact also - My experience was perfect
- Being made to feel welcome.
- If this was an ongoing thing. This exercise is only temporary which limits the help I can receive. I suffer from schizoaffective disorder. And have trouble coping with some things, or making the right choices. So what happens when my time runs out here. I don’t receive the help I need.
Western Victoria PHN

APMHA has been commissioned by Western Victoria PHN since 2016 to deliver the Psychological Therapy Service (PTS) and the Older Minds program (Supporting clients in residential aged care) for the last 3 years.
In April 2022, APMHA expanded the PTS program with extended funding to enable after hours services. This has been a fantastic additional opportunity as it supports the clinicians to provide more flexible service delivery to clients across the region.
We would like to thank our amazing workforce of 25 subcontractors and our partner Pritchard Health who have supported our clients and each other through COVID and program changes. We would also like to make special mention to those who have contributed to our Older Minds program as these clinicians have had to be extremely flexible, patient and considerate of all the changes presented to the Aged Care sector over the last 12 months, especially through COVID.
Thanks to our dedicated WVPHN workforce and our amazing central intake team, this financial year we have:

We would also like to thank WVPHN’s Referral Point Team and additional program support workers for their collaboration and support through delivering the program through another year of COVID and ongoing changes.
More about the programs:
PTS services target people with mild to moderate mental health issues, who may benefit from short term psychological therapy.
PTS: Includes specialist services to Children and Suicide Prevention . 471 individual clients have received 2460 sessions.
PTS After Hours: New funded program which commenced in April 2022 to deliver PTS after hours, allow our clinicians to be paid at a higher rate per session delivered outside of business hours, which in turn allows for more flexibility service options.
PTS Older Minds in RACF: Allows residents of Aged Care Facilities to receive inreach counselling. 91 individual residents received 586 sessions.
“I was able to use what I learned from the sessions which really helped me”
“The best thing about my experience with the service is that I get one hour of face to face sessions.”
“I got the help I need always, my clinician always helps me through my situations. I’ve never had a counsellor like that”
Staff Wellbeing Access Program (SWAP)
SWAP for RACFs

Swapping the focus to you – the RACF workforce

NWMPHN commissioned APMHA to provide a low intensity mental health in-reach program dedicated to staff employed in residential aged care facilities (RACFs) across the NWMPHN region.
The NWMPHN program key program objectives are to: build RACF workforce mental health literacy, promote help seeking behaviours and increase access to psychological intervention services delivered by the PHN (and other external services) such as HeadToHealth, CareInMind etc.
The APMHA Staff Wellbeing Access Program (known as SWAP) was initially established as a direct response to the COVID 19 (ALPHA variant) which occurred throughout 2020 and the consequential impact this directly had on the RACF workforce in the region. NWMPHN initiated the mental health response to support the workforce through Jan-June 2021. The SWAP program funding was then expanded for a further 15 months due to the emergence of Delta and Omnicron and the direct ongoing impact this was having on RACFs and their workforce now and into the longer term.
NWMPHN as funders, allowed for the SWAP program to be flexible. The collaboration and close working relationship allowed the SWAP program to remain innovative through each variant and lockdown and provided real-time in depth understanding of what the RACF workforce were and are facing day to day. Our clinical expertise has informed the methodology of the SWAP program design, which led to carefully developing a mental health program that was able to respond to the ever-changing climate of the COVID 19.
The impact of COVID 19 (Alpha) on the RACF workforce was wide ranging and the SWAP team were confronted with an environment that was unique to a typical disaster mental health response. The issues faced by RACFs included the outcomes from the Royal Commission into Aged Care, the ongoing negative media focus, the requirement of quick adaptation of RACFs to their work practices, roles and intensity that a mostly non-clinical workforce had to respond to through infection control measures, PPE, lockdowns, resident isolation and residents’ safety, whilst managing increasing frustration and anxiety with families. Although the SWAP Team employed a disaster response methodology – what became apparent is that this disaster was not going to end any time soon (unlike a bushfire).
The SWAP team members over many years have had significant experience in working in natural disasters and the relative stages of the typical mental health response: ie: acute / crisis stage, response stage, recovery stage, and rebuilding stage.
What was (and still is) clear, is that RACFs are in a continual phase of “acute response” and not able to focus on recovery. Each time there is a glimmer of movement out of the response phase, another wave and variant emerge, plunging the RACFs back into the acute response phase. Some 2 years on, response is ongoing.
In mid-2021, the Delta variant hit Australia and with this came a second wave of lockdowns for RACFs and unfortunately a second wave of COVID positive cases and deaths.
The RACF workforce have been in a constant state of hypervigilance, with little relief in sight. The palpable exhaustion and building moral distress is significant. Moral stress and distress is causing internal conflict and dilemmas for the workforce, on the way they would naturally provide care for their residents, and it is taking its toll on both staff and residents.
Since the commencement of the SWAP program, the differing COVID 19 variants have each had a public health response that impacted on SWAP’s ability to deliver the SWAP program as originally intended. The SWAP Team have needed to remain flexible in their approach to support the cumulative trauma, stress and exhaustion experienced by the RACF Aged Care Workforce. We have created multiple contingencies plans so that we could deliver the SWAP program regardless of lockdowns and impact of the Pandemic.
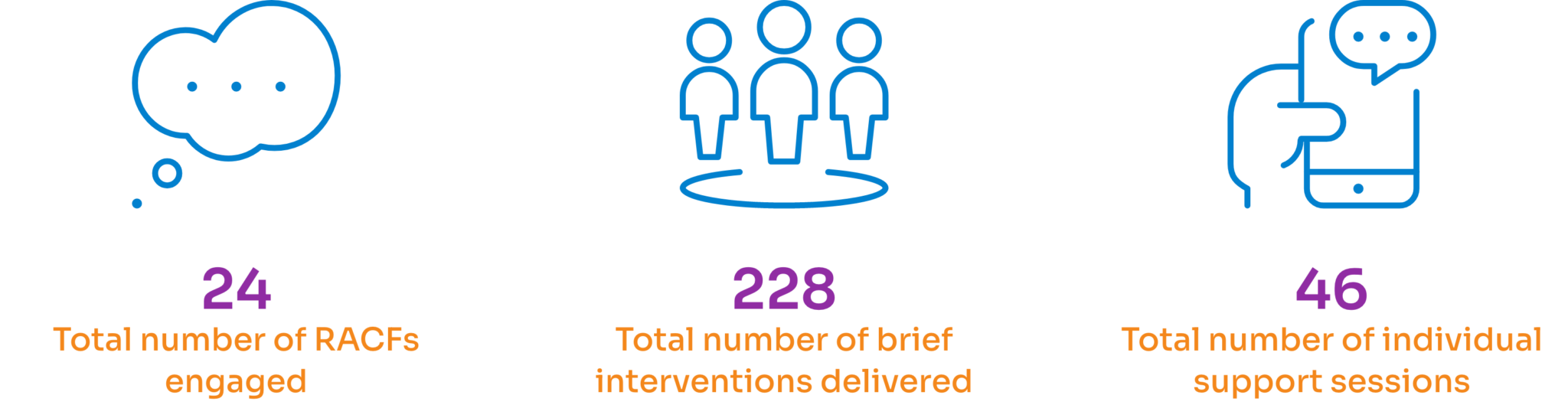
The Final report is in draft, however we are able to share our initial data:
- 24 RACFs out of 61 were engaged in the program.
- 15 RACFs participated in site visits, enabling the delivery of 43 face to face wellbeing support sessions to staff with 272 RACF staff participating.
- Of the 15 RACF’s that we have visited we have completed multiple return visits.
- 46 individual RACF staff members received direct support and navigation to ongoing counselling services.
- 228 brief interventions occurred during the site visits and the provision of SWAP showbags which included all the SWAP collateral, stress balls, herbal teas and other goodies. The SWAP showbags were so appreciated that many RACF’s provided each new staff member a SWAP showbag as part of their RACF new staff orientation program.
- We were able to deliver specific Management / Leadership wellbeing sessions either as a group or individually.
- Tailored collateral was developed focusing on Grief, Moral Stress, Anxiety, Depression, Alcohol and other Substances, Self Care, Anger, and SWAP promotional flyers and postcards for distribution.
- 100% of RACFs received monthly emails, webinar links and collateral for distribution to their workforce.
- A dedicated private RACF SWAP facebook page was established enabling further promotion of mental health messaging and links. The page now has 40 members in with 94 posts on supportive mental health information.
- A dedicated APMHA webpage was developed on the APMHA website providing links and resources for the workforce.
- 11 Webinars were recorded and links distributed via our email distribution list, facebook page and website.
“This was such a valuable talk as I know I am not on my own now.”
Central and Eastern Sydney PHN

APMHA has been commissioned by Central and Eastern Sydney PHN to deliver the Psychological Support Service (PSS) for the last 6 years. Through this time we have seen many changes, however the last 12 months have been one of the most challenging and busiest years.
We would like to thank our amazing workforce of 61 subcontractors who have supported our clients and each other through COVID, disaster response for floods and helped us pilot much needed inreach services to our elderly population.
Thanks to our dedicated CESPHN workforce and our amazing central intake team.

We would also like to thank CESPHN Mental Health Team for their collaboration and support through delivering the program through another year of COVID and ongoing changes.
More about the program:
PSS provides free short term face-to-face, or via telehealth, psychological service to people experiencing mild to moderate mental health concerns. This service includes provisional pathways, allowing clients to access services before they get assessed by their General Practitioner.
This service targets people experiencing Mild to Moderate mental health concerns, who may benefit from short term treatment. This service includes provisional pathways, allowing clients to access services before they get assessed by their General Practitioner.
This service is available throughout the Central and Eastern Sydney PHN region and aligns with a stepped, needs-based primary health care approach, also known as a Stepped Mental Health Model of Care. Clients who live, work, go to school, or see their GP in the Central and Eastern Sydney region may be eligible for this service.
Client Feedback:
“Validation with the empowerment to discover things for myself, but also the guidance when I couldn’t.”
“How welcoming and non-judgemental my Clinician was. I have been able to gain so much knowledge and understanding around what I’m actually experiencing without feeling like I am being diagnosed or put in to a box. She helps me rationalise my experiences, gives me vocabulary around topics that adds and deepens my understanding/awareness and enables me to view things from a more positive frame of mind. I’m very grateful I’ve had the pleasure of working with her and it has really impacted my life for the better!”
“My son Matthews mental health professional was very helpful he was professional and supportive and helped my sons mental health.”
Subcontractor Feedback:
“I feel blessed to be one of the credentialled mental health nurses providing care with the support of the team at APMHA and CESPHN. These organisations prove time and time again that to provide the best services for each client and strongly hold the client wellbeing as the foremost priority. The allocations teams at APMHA have taken time to know my skills and interests and have been totally supportive with appropriate referrals, information, and capacity changes. The management are very approachable and have provided expert guidance which has been invaluable as I set up a private practice, and continue to develop. It is refreshing to be supported by a Finance team who are dedicated to make sure the payments are correct, and respond to my embarrassing errors with efficiency and kindness. I feel extremely supportive and I feel very valued by the whole team. Thank you all!”
-S.G
South Western Sydney PHN



South Western Sydney PHN contracted APMHA to deliver the Credentialed Mental Health Nursing (CMHN) Service commencing 1 July 2021. We partnered with Inshirah – Nurse Practitioner Amanda Butt to provide leadership and support to local credentialed mental health nurses.
The CMHN service workforce includes seven very experienced and highly qualified Credentialed Mental Health Nurses who provide services to clients with more complex and enduring mental health issues across SWSPHN region. Allocation is filtered to our clinical intake team via SWSPHN.
This service is available throughout the South Western Sydney PHN region and aligns with a stepped, needs-based primary health care approach, also known as a Stepped Mental Health Model of Care.
The service commences through APMHA on 1 July 2021, with an establishment period during May & June of 2021.
We have enjoyed taking on this new program and working collaboratively with the CMH Nurses and would like to thank them for all the dedicated and amazing work they provide.
About the program:
The CMHNS provides support to Clients with a severe and complex mental illness through clinicians who are Credentialed Mental Health Nurses (CMHNs).
The CMHN provide the following services:
- Establish a therapeutic relationship with Clients;
- Close liaison and support for family and carers;
- Mental health assessment, treatment and monitoring;
- Collaboration, networking, liaison, and where necessary, managing referrals to other services and health professionals;
- Contribution to care planning and management including medication management, treatment and Psychotherapies; and
- Psychoeducation and provision of health promotion information
- Psychological therapies
Clinical Care Coordination includes:
- Maintaining links and undertaking case conferencing with Psychiatrists and Allied Mental Health Professionals such as Psychologists, Social workers and Occupational Therapists (health professionals may be eligible to claim case conferencing items under MBS);
- Coordinating services for the Client in relation to GPs, Psychiatrists and Allied Health Professionals;
- Arranging access to interventions from other health professionals as required;
- Contributing to the planning and care management of the Client;
- Liaising with supplementary services, such as Allied Health services, psychosocial support services, NGOs and CMOs and Government Departments.
Providing Clinical Support and Sector Capacity Building:
- Building capabilities amongst GPs, Practice Nurses, Allied Health and other relevant health professionals in conducting clinical assessments and providing treatment advice, for example, formal mentoring or training processes with a focus on build confidence in supporting Clients with severe mental illness.
- Co-assessment with GPs, Allied Health and relevant professionals, advice on the mental health management and treatment, and recommendations on referral options.
- Secondary consultation to assist in developing treatment plans, discussion about clinical approaches, advice on therapeutic technique and education input as required by general practice or Allied Health Professionals.
NavSpace

NavSpace was funded through BRV to build the website and mobile app through the Bushfire Recovery Grants for Local Government Authorities and Community Service Organisations.
These grants were established to assist bushfire affected communities with their medium to long term recovery by providing funding to deliver projects and undertake activities aimed at community recovery, community development, community resilience and capacity building for the future.
In response to the 2019-20 Victorian Bushfires numerous services were funded to support community recovery and postvention support. Keeping track of all stakeholders and their service offerings involved in recovery efforts proved difficult. Directories quickly became out of date and something more long term was required.
The recovery and emotional wellbeing committees in the North East Regions outlined the need for a more strategic and longer term solution that can remain current and versatile in the ever-changing environment. COVID-19 created additional challenges in service offerings and responses, hence increasing the need for some form of online and smart phone directory which can stand the test of change and time.
APMHA HealthCare submitted a proposal to Bushfire Recovery Victoria to fund the development of this solution. The local Bushfire Recovery Victoria committees endorsed the proposal and worked collaboratively in its development over 2020-2021.
NavSpace is an online navigation guide to increase mental health and wellbeing support access in the North East region of Victoria. This website and smartphone web app has been developed to support ongoing community recovery and service response particularly relating to local disasters and COVID-19.

Navspace was officially launched on the 8th of October 2021.
Since the launch, there have been 4.1k site visitors with 3.2k meaningful user engagements.
NavSpace is also a smartphone web app which can be saved for use whenever needed!
Alaya House – Wellbeing Hubs
Alaya House is the name of our new wellbeing hubs. Where we have created a welcoming, safe and supportive space for community members of all ages, who require specialised support for mental health issues, drug and alcohol issues, and psycho-social disability.
In 2019, APMHA realised our dream to establish our first mental health wellbeing hub located in Shepparton, Victoria. Our aim was to create a hub which focuses on wellness, recovery and supporting people to live a full and contributing life as determined by them. Through this established hub, we have created a physical presence in the region and a holistic team approach with our various funded local mental health services and workforce. In 2021, we opened our second hub in Footscray, Melbourne.
Alaya House Shepparton

Our Shepparton hub includes:
- High quality mental health services Psychological Therapy Services (PTS), Clinical Care Coordination (PMHCC), HeadtoHealth Program, NavLife Bupa Program and Medicare billing services.
- General Practice services
- Group therapy and psychosocial education programs for clients.
- Workforce and community education and training delivered through our training room.
Client comments on Alaya House Shepparton:
“I am always welcomed at the door with a smile. It is great”
- I felt very welcomed and in a safe environment to open up
- Relaxed and welcomed with a smile – I felt calmed.
- Every staff member we encountered were amazing! Always pleasant and polite
Alaya House in Melbourne
Over the last few years, APMHA has had 3 different Melbourne office locations for our main headquarters.
Our first site was in Flemington and housed us for 3 years, however as our team grew, so did our need to move to a larger facility.
North Melbourne was our second site, which was perfect for our needs, however four months after moving in, COVID hit Victoria and our office location was the first to go into lockdown in March 2020. A decision was made to decommission this space until we further understood what lay ahead for Melbourne through COVID. All our staff were moved to Working From Home arrangements.
In July 2021, APMHA opened our third site in Footscray. Where our general staff and clinicians could work collaboratively in the delivery of APMHA services. While everyone at APMHA has enjoyed bringing the Melbourne team together again, the pandemic continued and our staff were moved back to WFH arrangements on and off. We decided to once again close our Melbourne office, and WFH is now ongoing, with monthly team meetings and training days for now.
Our aim is to reopen a Melbourne office in 2023, and the Executive Team are currently scoping options that are first for purpose and more suited to our needs.
“Thank you for all of your assistance over the last year or so. You have been extremely courteous, approachable and professional and it was a pleasure communicating with you.”
GP Clinic
APMHA has been very fortunate to recruit two GPs, who provide holistic services targeting mental health, eating disorders, physical health, sexual health, youth health and mental health.
Dr. Michal Moon and Dr. Louise Bradley attend the practice in Shepparton on a rotating roster. Dr. Moon finished his time with us at the end of June, and we are very thankful for the ongoing fortnightly services of Dr. Bradley.
Through 21-22, our part time GP practice has provide services to 80 patients and delivered to 405 consultations.
Positive Workplace Program
Positive Workplace Program – Employee Assistance Program (EAP)
Creating mentally healthy workplaces.
At APMHA, we believe your employees are your most valuable asset. These are the people who will ultimately determine the success or failure of your company. Supporting your workforce to be their very best at work is the first step in creating the perfect environment for future growth – individually and as a company.
That is why we have developed the Positive Workplace Program (PWP) – to help Executive Teams to infuse wellbeing into the heart of your organisation. We do this by enabling each and every person to operate at their fullest potential. After all, every problem contains the seed of its own solution – and by empowering people to help themselves, you build a happy, healthy workforce. And when you unlock human potential, powerful business outcomes follow.
Our adaptable program covers resilience-building education and training relating to the importance of healthy eating, positive lifestyle choices and exercise, team-building programs, and comprehensive mental health support services. Together, it becomes a game-changing workplace program shaped to your organisation’s unique wellbeing needs.
We currently have four contracted EAP private organisations and have delivered 65 sessions to 9 employees.

Workforce Training and Support
APMHA have funded or delivered various training programs for our workforce and GP referrers. These included:
- 7 workforce COVID support webinars
- 11 SWAP RACF webinars
- 4 GP and practice staff – Mental Health in General Practice Webinars
- APNA and 3 PHN webinars for practice staff, GPs and MPs
- 1 x 6 hour Advance Suicide Risk Assessment and Prevention training with Alfred Mental & Addiction Health
- 2 x 6 hour workshops on Aboriginal Cultural Perspectives Training with Ochre & Salt Pty Ltd
- 1 x self paced training pilot to support CALD clients
- 6 FIXUS training webinars
- Supervision – Individual session provided by APMHA = 65
- Group supervision sessions provided by APMHA = 20 to 10 clinicians
Comments from Training held:
- Really appreciated the combination of modules, but in particular the zoom session hearing personal experiences and bringing all the theory to life in a vibrant and interactive way
- A lovely facilitator Very open and approachable Thank you for sharing your stories and knowledge with us
- The importance of employing curiosity and not knowing stance in developing a therapeutic alliance
- This training was amazing thank you, I really appreciate the encouragement of further readings and suggestions provided which I will be looking into!
- A very useful workshop – thank you. I actually used the skills on a real client later that afternoon
- I really enjoyed the workshop, engaging and well presented, I realised how much I did know and added to my knowledge base
“The presenters clear and extensive knowledge base was much broader than any previous cultural training I have attended. Gave a much more insightful aspect to consider.”
Supervision Supervisor
Almost two years ago, I joined APMHA. As a consultant, I was given the opportunity to work with a wide range of clients in several programs. At that stage it was unclear as to whether or not clients would be willing to accept psychological services provided either by various methods on the internet, or by telephone. However, within a couple of months Covid was identified in Australia for the first time, and it became clear quite quickly that f2f counselling would be difficult to provide safely. This led to the understanding that online and telephone work would need to become the main platforms for provision of services until Covid could be managed or eradicated.
This major shift in service provision meant I was able to accept and work with clients from a wide range of socio economic backgrounds, varying age groups, and ethnicity. Like many clinicians, I found it took a while to become comfortable with using Zoom, and learn how to adapt to observe client nuances and body language in an online environment, and most importantly, build trust and make a connection. Nevertheless, I began to enjoy the challenges of working remotely and took more clients as the need increased.
At the same time, I was offered the opportunity to take on a Supervision role with some of the staff and other Consultants. I had been doing this role in several other organisations for some years, and always enjoyed it with both its’ various challenges, and the benefits of it that I observed over time in many of those I supervised. This was evidenced from research that has shown that good supervision correlates with job satisfaction (Hawkins, & Shohet, 2001). It has also been found by other researchers that Supervision is an essential component to support the professional demands of the continuing education of Clinicians, and also “when faced with ethical or clinical dilemmas”. (Corey, Corey, & Callanan, 2007, p.360)
My own experience is that Supervision is a very important form of support, where we can focus on our own challenges as a Clinician, reflect on things that have worked well, and have our supervisor share some ideas and examples of alternative strategies when working with the clients. Additionally, Supervision forms part of our continual learning and development. This can involve more effectively managing our workload and challenging and revising our own ways of coping.
Observing the Supervisee’s own mental health, and particularly identifying the early stages of burnout has been a very important aspect of Supervision, particularly during the first two years of Covid, when Clinicians, as well as clients, were experiencing the enormous stressors linked to the recurring lockdowns and the ongoing uncertainty about the future. As A Supervisor, I am aware I also need to be cognisant at all times that if I am supporting Clinicians to consistently assess their own self and their practice, ethically it is essential that I am doing the same.
I am very grateful to AHPMA, a dynamic and supportive organisation, for giving me the opportunity to work with some of the clients who have sought our support during times of great difficulty. I also feel privileged that I have had the opportunity to work both individually and in groups with the many experienced and caring Clinicians who have shared their journey with me over the last two years, through such a difficult and ever changing period of clinical practice.
– Dr Anne Pratt
Hayespratt Consulting
