Our National Achievements

Our Stories
APMHA has a workforce of 135+ highly trained mental health clinicians who provide mental health services to vulnerable communities. Working under strict program funding requires dedication and commitment alongside significant reporting and data entry. Our clinicians are the backbone of our company – here are their stories.
Theresa Corin - Employee Assistance Program
I have been working with the APMHA as a subcontractor for over seven years now and continue to appreciate the service focussed ethos of this organisation and the enduring, collaborative relationships I have developed with its personnel.
Last year, in my capacity as a Psychologist, I offered counselling intervention to a number of individuals who had self referred through their organisations EAP schemes for an array of issues. Irrespective of their presenting problems, individuals were encouraged to move from a state of inertia and overwhelm to pro active problem solving, implementing both behavioural and cognitive strategies to increase their functioning and sense of wellbeing.
Whilst this counselling was often brief in its duration, clients anecdotal reports and post intervention assessments generally indicated significant, positive gains having been made to their mental health and corresponding functioning both in and outside of the workplace.
Theresa Corin MAPS
Counselling Psychologist
Dr Jane Oakes - Murray PHN Programs
I’ve been collaborating with APMHA for about two years now, serving as a telehealth clinician under subcontract. This platform has provided a fantastic opportunity for my clients to connect with me, right from the comfort of their own homes. It’s been a positive experience for many, eliminating the need for childcare arrangements or the difficulty of commuting to appointments. For those with busy work schedules, the convenience of telehealth has also been greatly appreciated. It has streamlined the therapeutic process, allowing us to work on their treatment plans effectively.
Working with APMHA has been a truly rewarding experience. Despite my role as a subcontractor, I’ve found the team to be exceptionally supportive and responsive. The atmosphere within the organisation is a positive one, fostering camaraderie and radiating a welcoming vibe whenever we communicate. Whenever I’ve needed more clients or additional sessions for my existing ones, the allocation team has been swift in addressing these requests. The commitment to meticulous attention to detail and rigorous clinical governance processes ensures that best practices are consistently upheld for the clients who entrust their care to APMHA. It’s evident that the well-being of our clients is a top priority, and this dedication shines through in every interaction between the team and clinicians.
As a practitioner grounded in evidence-based approaches, I’m truly grateful to be part of an organisation that prioritises the best possible care for clients and their treatment plans. Witnessing our clients progress towards their therapy goals and ultimately experiencing an improved quality of life and well-being has been an incredibly fulfilling aspect of my work at APMHA.
Vicky Northe - Murray PHN Programs
It is a pleasure to work for APMHA as this service provider as it provides flexibility with the support of being part of a team with backup and supportive safety measures for clients and staff.
I am an Accredited Mental Health Social Worker with 20+ years of experience in New Zealand and Australia. For most of my career, I have worked within several Public Mental Health Services in Child, Adolescent and Family Mental Health, Maternal Mental Health, and Adult Mental Health, plus running a State-wide Mental Health and Gambling Harm Service.
COVID globally changed the way we deliver therapy to the community. At a local level, where lockdowns created increased community stress, there was a need for a flexible approach to working with people and society as we could not simply do ‘business as usual’.
Pre-COVID, when possible, I always strived to meet people face-to-face in the community where they lived. I was lucky enough to run a service where I could travel around Victoria to see people in their community rather than make clients drive to Melbourne. I believed that providing face-to-face intervention in a person’s local environment could increase engagement, assist in collaboration of service delivery and assist in decreasing client burden, such as reducing the
Starting my working career in regional New Zealand, I was used to a more mobile and multitasking approach to service delivery, where one worker may need to develop skills in several areas. When I moved to Melbourne, my work was often more place-based or speciality-specific due to increased resources. Each has advances and disadvantages in focus, diversity and sharing of knowledge. The state-wide program experience enabled me to reconnect with regional and rural areas where everyone has to pull together and become creative to ‘get the job done’, often with limited resources, staff availability, or access to specialist services.
COVID allowed me and workers within my ecosystem to ‘do work differently’. We were forced to utilise the technical advances available, and policy changes created an authorising environment to ensure it could happen. More importantly, the community became more adept at using technology to access services, which was, on reflection, the reason for its success.
The move into this new work methodology didn’t happen without questions. For years, we had held up confidentiality and safe connectivity issues as a reason for not engaging with it. When forced to look at these barriers as a community of services, we were able to iron out these concerns very quickly, and people got used to using online communication tools. As the community began to use the tools in everyday life with family and friends, it further strengthened their trust, and we even started to see examples of online etiquette emerge.
As we head towards the end of 2023, I believe people have increased confidence in Telehealth services. As an Accredited Mental Health Social Worker, Telehealth can be as effective and helpful as face-to-face intervention.
There are areas of therapy where Telehealth has proven a considerable advantage. With social anxiety, agoraphobia or severe depression, for example, Telehealth can now be used as a bridging tool as people can access therapy as they do not need to leave the house and by commencing treatment for mental health problems that may decrease motivation and ability to face the world outside we can work together to take the following steps. We may also be able to use the technology to be with people as they assume their first venture outside, and we can address any panic right there with the person, thereby increasing their confidence and courage to repeat these changes.
In regional and rural places, it addresses both the tyranny of distance and the rising cost of fuel, both of which had been barriers to seeking support.
I have moved from working at a tertiary health level to a primary mental health service. This move has provided me with career satisfaction with the knowledge that my skills may help to avoid an increase in mental health struggles that may lead to an increase in distress and use of hospital services. Preventing this next level of care means that people can start feeling better without the increased pain and trauma of a possible hospital admission.
Working for APMHA allows private practitioners to feel supported in their work, as the service provides:
· Good levels of support and structure.
· Clear intake and accessibility to several programs.
· Clients have the option of face-to-face or Telehealth.
· The authorisation to use a broad range of therapy models to suit each person’s unique situation as required.
· An increased capacity to manage and support risk when people are facing struggles and vulnerabilities.
· The knowledge that as a contractor, support is only a phone call away with good community networks.
· More recently, when working with people impacted by natural disasters, it was advantageous to have APMHA knowledge and the ability to make sure that communities maintained access to support they may require and monitor service delivery to flood-affected Families.
In closing, I am happy and honoured to be part of the APMHA team. I have now begun planning to visit some of the regional areas to ensure I stay informed of the local environment and maintain community networks. I look forward to starting with a visit to Shepparton.
Diane Garcia - South Western Sydney PHN Program
I commenced with APMHA in August 2022 as a subcontractor. I currently provide both face to face and telehealth. The majority of my appointments are face to face both centre based and home visits.
Working under the SWSPH’s CMHN Program allows me to collaborate with various referrers, this includes but is not limited to GP’s, Education, Public Health Services, NGO’s and DCJ. In addition, it provides me the opportunity to create partnerships with services that compliment the care I provide consumers. This includes Psychiatry, Peer Support, Psychosocial Support, Drug and Alcohol services and Disability Support. The shared care model promoted by SWSPHN allows for a holistic approach for consumers where services may be limited to provide specific care.
Being based at Community Links (SWSPHN Program) in Tahmoor is an absolute bonus as I have learnt about the amazing services they have to offer, in turn I have been able to refer clients to their programs. TheThe stepped care model provides ongoing support for consumers who are ready to be discharged from the CMHN Program and also for consumers who require more intensive support who can be stepped up to the CMHN Program for appropriate levels of mental health support.
The CMHN Program offers my clients experience, knowledge and evidence based support from Nurses who apply individualised care. The CMHN Program offers care coordination and monitoring of risk and resiliency factors. As a CMHN, I provide therapy targeted to specific areas of the client’s needs and goals. Being able to provide education and service resources to clients sets the foundation of gaining insight to their mental health recovery journey. The Program provides a safe space to have difficult conversations about their challenges without judgement and with empathy. Being able to engage clients via telehealth, centre-based, community based and home visits allows flexibility in the CMHN Program which improves the overall access to care for clients who may be experiencing barriers to receiving care.
The CMHN Program provides a free service which gives clients a relief from financial strain for a period of 1-2 years. This closes the gap for clients who do not meet the criteria for Public Mental Health Service and cannot meet the expenses for Private Psychological Services.
Working for APMHA has allowed me to grow as a clinician. From working in a multidisciplinary team for over 10 years to working as a sole clinician in my private practice, I continue to feel supported by the clinical staff from AMPHA, other CMHN clinicians and SWSPHN Programs. As a sole clinician, I feel confident in taking leave as APMHA provides interim re-allocation for clients who may need ongoing support in my absence, this makes me feel part of a team and reassured that client’s will not be left without support.
APMHA has a solid process with intake which allows me to start my recovery journey with clients at ease. With referrals, APMHA is respectful of my scope of practice and capacity to accept and decline new referrals. APMHA has provided me with the opportunity to engage in group supervision, training and clinical support with difficult clients. Staff from APMHA have clinical backgrounds which creates understanding in the support we provide clients, this includes having approved extended client sessions, increased clinical support for clients and being involved in complex care-coordination. APMHA has an open door policy which makes me comfortable to reach out when seeking support whether it be clinical or non-clinical.
Terence Kuun - Central and Eastern Sydney Program
My name is Terence Kuun, and I work under CESPHN’s PSS program. I would like to tell you a bit about the program, as well as about experiences of working with CESPHN and APMHA.
I began working with APMHA in 2016, and I have primarily worked under the PSS program, although I have also done some work under PTS, which is a variation based in Victoria. I subcontract, which works well for me, as I like being in private practice and doing a variety of work.
If you have not heard about the PSS program, it is a funding stream parallel to Medicare, provided by CESPHN. There are different versions operating under different PHNs throughout Sydney and beyond, and they have different names and different configurations. By contrast, Medicare is standard and is federally administered. CESPHN’s PSS program provides sessions for clients experiencing mild to moderate mental health issues, and for whom there may be barriers to accessing Medicare sessions. Some examples are those with low income, Aboriginal and Torres Strait Islander people, young people, people from multicultural backgrounds. Clients are not charged a gap fee, and there are more sessions available than under Medicare. It is a very inclusive program, and I see a wide range of people under this program.
Initially, all of my PSS sessions took place face to face, but during the pandemic, the bulk of my work was Telehealth. Over the last year, my work has again primarily taken place face to face, but about a quarter of my sessions are still Telehealth. Clients choose this option for several reason, and only a small number are motivated by concerns about infection risk. Most choose this option as they have limited flexibility with their everyday responsibilities and routines. I like this option as it removes obstacles that in some cases would mean that clients would have to forfeit mental health care.
I really enjoy working under PSS funding. It has changed somewhat over the years, but it has always been a good system. Recent changes have increased client access to sessions, and I think it is now quite a generous system. Treatment is not indefinite, but the program is flexible enough to meet individual needs. There is provision for additional sessions under exceptional circumstances, and clients are able to have access to a second round of treatment if necessary. While PSS treatment cannot be rolled over indefinitely, the program really does allow for a solid enough chunk of therapy to make a real difference to someone in distress. In rough terms, clients can comfortably have fortnightly sessions for about a year, and this treatment is at no cost to them. This is often enough to deal with presenting issues, or it may transition to Medicare funding. There are also cases where we have used the time to apply for NDIS funding for longer. As I said previously, there is also the option of a second round of treatment for some clients. All in all, I think the program works well.
Under CESPHN funding, I also do Suicide Prevention sessions. This program is also very generous, allowing for very intensive client contact over a limited period. These sessions are in addition to any other session that the client has accessed, and there is sufficient flexibility to step clients up and down when needed.
In my opinion, PSS sessions are also adequately remunerated. No gap fee is permitted, but I think the rate is fair. As with Medicare, it can be slightly frustrating that practitioners cannot charge when clients do not attend, but in my practice, this has not ever been a significant issue.
I like the PSS program, and I also really like the organisation that implements it. I find CESPHN a supportive organization with good systems and a great culture. There are times when I have to contact them telephonically or by email, and staff members have always been friendly, helpful and efficient. I have developed ongoing friendly relationships with several staff members, and I have always felt very comfortable and supported when seeking assistance from CESPHN. CESPHN is also a very good organisation with regard to training and professional development for practitioners. They provide a lot of free training, and this training is of a very high standard. Throughout my career, I have paid many thousands of dollars on courses, and much of the best training I have received was provided by CESPHN at no cost. Training has often taken place at the CESPHN offices, and this is a very welcoming environment.
As I said above, I subcontract to APMHA, and it is through APMHA that I work with CESPHN clients. To put it in a nutshell, APMHA is a great organization to work with. I have consistently seen how the organisation is highly committed to both client and contractor wellbeing. While it is obviously a business, it is definitely not just about the bottom line. Their systems are very good, and they deliver high-quality services in a manner that is both friendly and efficient. The APMHA team consists of a wonderful group of people who are warm, supportive and collaborative. I have had to request assistance with a range of issues over the years, and the APMHA team have always been lovely to work with. As a result, I have developed very nice personal connections with a whole lot of people in the organisation.
APMHA is very generous with the time and resources that they provide to contractors. Contractors are well-supported clinically, with regular free supervision sessions available. Contractors are also given a lot of support regarding professional development. APMHA is proactive in providing in-house professional development and training, organizing free external training and notifying staff of other external training that is available.
I really do think that the APMHA is a unique and special organization that really demonstrates what is possible to achieve. I cannot overstate how people-focused it is, and I can honestly say that it has been a very special experience to be working with such a supportive network of people. Not only do I feel very fortunate to be a contractor to the APMHA, but I can honestly say that I genuinely feel like a much-included part of the APMHA team.
I really encourage anyone who is interested to consider doing PSS work with APMHA and CESPHN. I have had my share of horrendous, disorganised, toxic organisations, so I do have a bit of a cynical take on organisations in general. However, I want to say that I really am very happy doing the work that I currently do, and to be working with two organisations that really do function well and really do care about people. This is not something to be taken for granted, and I love that I am able to share with you that this reality does actually exist, and it may be a possibility for you to explore!
Nabill Zafir - Central and Eastern Sydney Program
I started working with APMHA in 2021 as a subcontractor. I provide both telehealth and face to face services.
I enjoy working within the PSS program funded by CESPHN, the program offers tangible and meaningful value to clients and helps achieve appropriate health outcomes. Clients have expressed their gratitude about being able to be allocated to a clinician in a timely manner and often describe the point of referral to allocation as seasonable. One of the main benefits of the program is accessibility; the program allows short-term psychological interventions for clients who are experiencing financial hardship or experience other barriers to psychological support.
Working alongside APMHA has been a positive experience. The allocations team are very helpful and are a significant support. APMHA are inclusive and they support your professional develop and working needs. They offer opportunities for learning and advancement which has been invaluable to my career progression.
Sharyn Amos - SWAP and North Western Melbourne Program
I have worked with APMHA for years, but I have left and come back a few times – like a revolving door and each time got a going away present…
I provide both with Older Minds is always face to face.
It has been challenging as the COVID pandemic had such an impact on RACF’s and I believe residents and staff are still facing the post COVID pandemic, Royal Commission challenge. All RACF’s need our support and care as they still work hard to ensure that our valued Older members of our community are supported and loved in this current challenging environment
The program offers access to a Mental Health Workforce that becomes a part of the fabric of the RACF. Older Minds offer counselling, secondary consultation, education for residents, family members and staff.
I have worked in many workplaces and worked with the most challenging clients, residents and in sometimes most challenging environments within Australia. This is the first time that I have experienced a workplace that aligns with my own philosophy of clinical work where if you look after clients, families and other members of APMHA then they have your back. As an older clinician who has seen so much darkness in the world of mental health it is a rare commodity that the workplace will actually support you when all you are doing is your work within the clinical governance framework that supports you.
Western Victoria PHN

Central and Eastern Sydney PHN

Murray PHN

North Western Melbourne PHN

South Western Sydney PHN

Employee Assistance Program

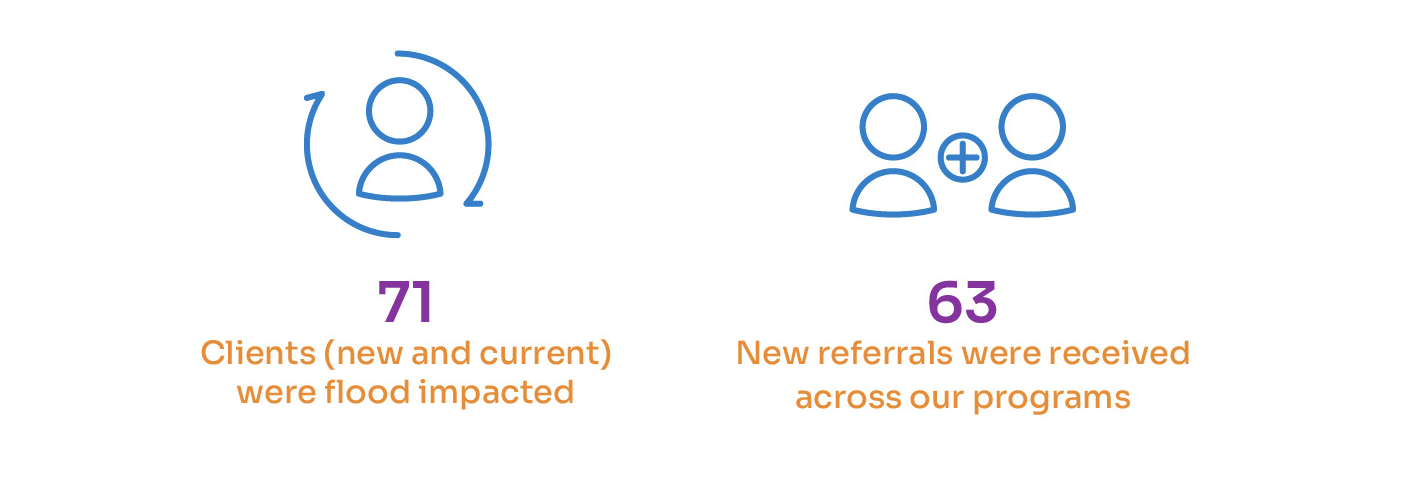
Floods – SWSPHN and Murray PHN
APMHA were one of the first responders to meet the mental health needs of people impacted by the floods in the Shepparton and surrounding areas, with our staff attending local community hubs, relief centres, aged care facilities, as well as out reaching to homes, as soon as it was safe to do so. All clients engaged with APMHA at that time were contacted to assess for flood impact and ascertain any need for support.