IAR Overview
Full implementation of the National Intake, Assessment & Referral Tool.
The Initial Assessment and Referral (IAR) Tool is a national tool used across all PHNs and State funded services. It was designed to assist service providers to assess a client’s needs and determine the level of care aligned to the most appropriate referral path or service.
The IAR is for:
- General Practitioners (GP) and other clinicians seeking to make referrals and guides selection of best fit of service the the client’s need
- APMHAs Intake team and workforce are also responsible for undertaking initial assessments and/or recommending the level of care required. Due to this all APMHA employees are training in IAR when they commence.
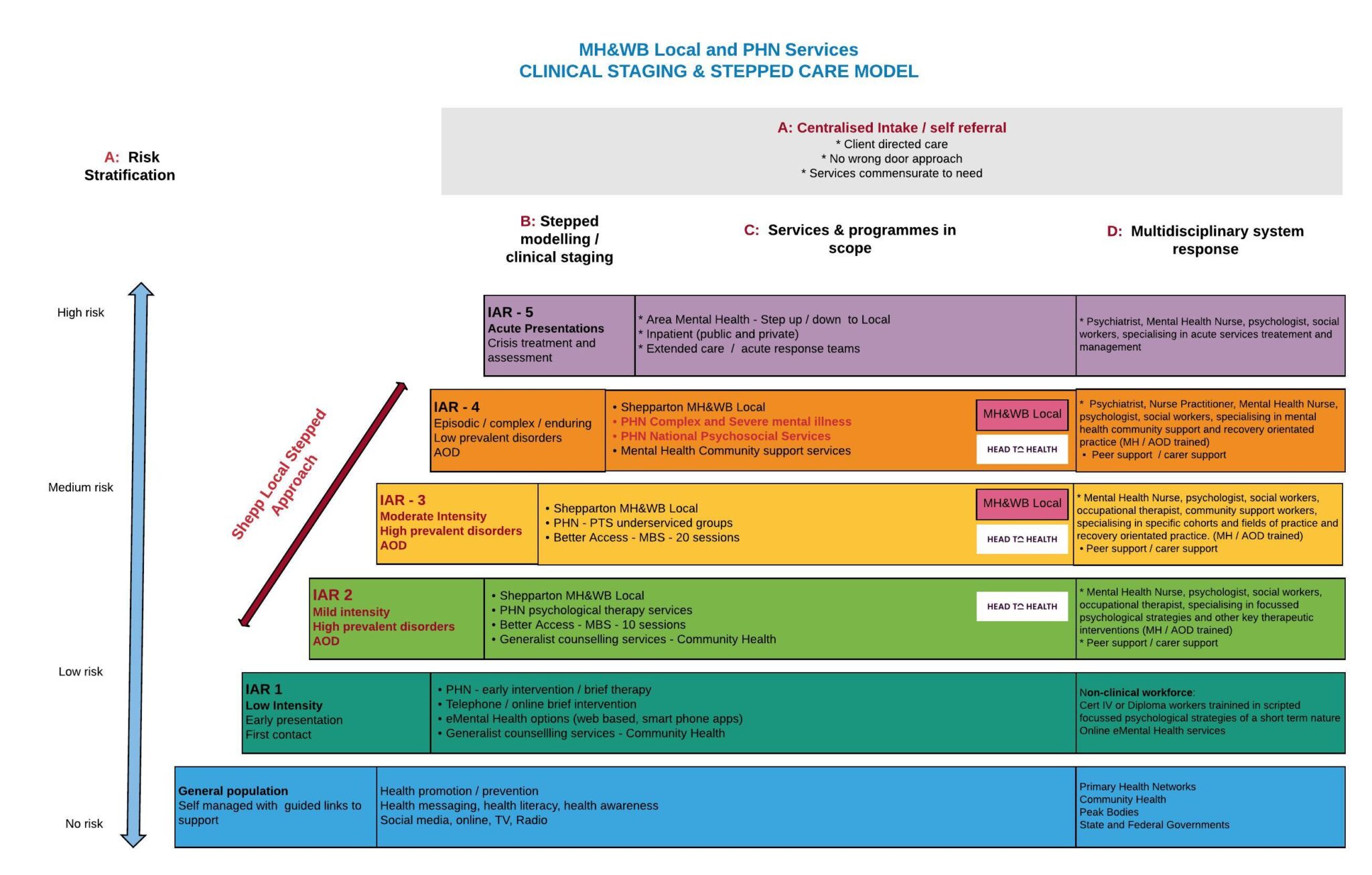
Our Stepped Care Approach
APMHA HealthCare has developed a Service Delivery Framework to reflect a Stepped Mental Health Model of care which sets out the strategic direction of the Company. In APMHAs stepped care model we:
- ensure clients receive care commensurate to need, this being determined by the IAR assessment on intake or at their first appointment.
- ensure person centered care which targets the needs of the individual and recognises that needs may change at any time
- work in strong collaboration and partnership with general practice, carers, and other stakeholders
- focus on the client’s trajectory for their determined recovery
- facilitates seamless transition of clients up / down, a stepped mental continuum whilst maintaining continuity of service provision.
Services we deliver under Stepped Care

- Central & Eastern Sydney PHN
- Murray PHN
- North Western Melbourne PHN
- South Western Sydney PHN
- Telehealth service provision with linkage to online services.
- Murray PHN
Level 3
- Murray PHN
- CESPHN
- NWMPHN

- SWSPHN
- Murray PHN
Vulnerable cohorts we support
Child Mental Health Services & groups
Refers to children who are aged between 0-12 years, who have, or are at risk of developing a behavioural / emotional / mental health disorder. These include:
- A child assessed as having definite or substantial signs and symptoms of an emerging mental health disorder, where this causes significant dysfunction in everyday life and/or
- A child at risk of developing a mental health disorder, where the child shows a number of signs and symptoms ( whether that be social, emotional or behavioural) and where the child’s developmental pathway is disrupted by their mental health clinician.
APMHA delivers Child focused mental health services to most regions, with Central and Eastern Sydney and Murray regions being the highest referral rates. In the Murray region we deliver both individual and group options to these clients.
Our Child clinicians are credentialed to provide services to children and are highly experienced.
Youth
Youth services refer to people aged between 13-25 who may benefit from psychological support. While Headspace also offers this service, APMHA often works with clients from this cohort who are transitioning out of Headspace or may not wish to join the Headspace service. APMHA provides services to young people across most service regions, with Central and Eastern Sydney having the highest referral rates for this cohort.
Aboriginal and Torres Strait Islander people
Through APMHA Services, Aboriginal and Torres Strait Islander people are able to access mental health services that are integrated, culturally appropriate and safe. Aboriginal and Torres Strait Islander services are designed to holistically meet the mental health and healing needs of this population group and are delivered by clinicians with additional training in Cultural Awareness. APMHA provides mental health support to Aboriginal and Torres Strait Islanders across all regions and prioritises training opportunities to all workforce.
Our clinicians are credentialed to provide services to Aboriginal & Torres Strait Islander communities and are highly experienced.
Culturally and Linguistically Diverse people
Many PHN Needs Assessments recoginise that access to psychological therapy can be impacted by low English proficiency, cultural stigma and limited support networks. Due to this, interpreter services are available throughout all APMHA Services and culturally appropriate clinicians are made available in all APMHA programs. APMHA also priortises training in this area, ensuring training is always available to clinicians.
Perinatal
Many of our PTS/PSS services prioritise this cohort as the national perinatal depression initiative (2013) recognised the need to improve prevention and early detection of antenatal and postnatal depression. APMHA continues to support this initiative through the Central and Eastern Sydney region and is currently working towards a pilot service in the Murray region.
Suicide Prevention Services
This service provides priority access for Individuals who have attempted, or are at risk of, suicide or self-harm or who have suicidal ideation and are already being managed in the primary health care setting. While APMHA works with the Suicide Prevention Services in most regions, this is not acute care and tends to focus more on reducing Suicide Ideation.
Residential Aged Care Facility (Older Minds)
This service allows residents of aged care facilities to access the psychological support available to others in the community. APMHA clinicians travel out to Residential Aged Care Facilities across Murray, Western Victoria and North Western Melbourne regions.
Employee Assistance Program (EAP)
Our tailored Employees Assistance Program (EAP) is a boutique service, offering organization employees specialist counseling and wellbeing support. It encompasses training, counseling and critical incident and wellbeing support. EAP is delivered by APMHAs a highly proficient, experienced and specialized accredited mental health workforce, which includes psychologists, mental health nurses, mental health occupational therapists and mental health social workers.
Head to Health decommissioning
On the 9th of March 2021, APMHA was funded by Murray PHN to rapidly establish one of 17 HeadtoHelp Hubs in Victoria as a direct result of the mental health and wellbeing impact from COVID in Victoria due to extended lockdowns. The HeadtoHelp Hubs were designed to provide high quality, evidence-based treatment, information, and support to people of any age who may be experiencing distress or mental ill health, and their families, carers, or support networks. The HeadtoHelp Hubs, were embedded in existing community settings and facilitated a holistic approach to care which addresses a broad range of social, physical, and emotional needs, especially during lockdowns and post lockdown periods in Victoria.
In early 2022, HeadtoHelp services across Victoria were rebranded to the new name HeadToHealth and further expanded to be available in all other States through PHN funding.
From January – June 2024, APMHA commenced decommissioning of the Shepparton and Seymour Hubs in preparation for transition to the Victorian State funded Mental Health and Wellbeing Locals under a Federal / State bipartisan agreement. The program closed in Shepparton and Seymour on 30.06.2024.





