Company Overview
APMHA HealthCare Ltd (APMHA) was established as a national Not-for-Profit company in July 2019 having evolved from Victorian Primary Mental Health Alliance Pty Ltd (est 2015). As a Not-for-Profit, our focus continues to be on vulnerable and under-serviced, priority populations.
APMHA provides intake, triage, allocations and clinical mental health services for a variety of funders through nominated program streams across Victoria and NSW. Our focus primarily evolves around primary mental health care.
Our funders include Primary Health Networks, State Governments, NDIA, MBS and others. Our partners include government, community health services, rural hospitals, PHNs, tertiary services, private mental health practitioners, community and private sector organisations and various peak bodies.
We have 135 dedicated clinicians – a highly experienced and reliable workforce engaged through a hybrid model with a mix of employed and subcontractor clinicians. Our locations are numerous across Victoria and NSW within our funded regions.
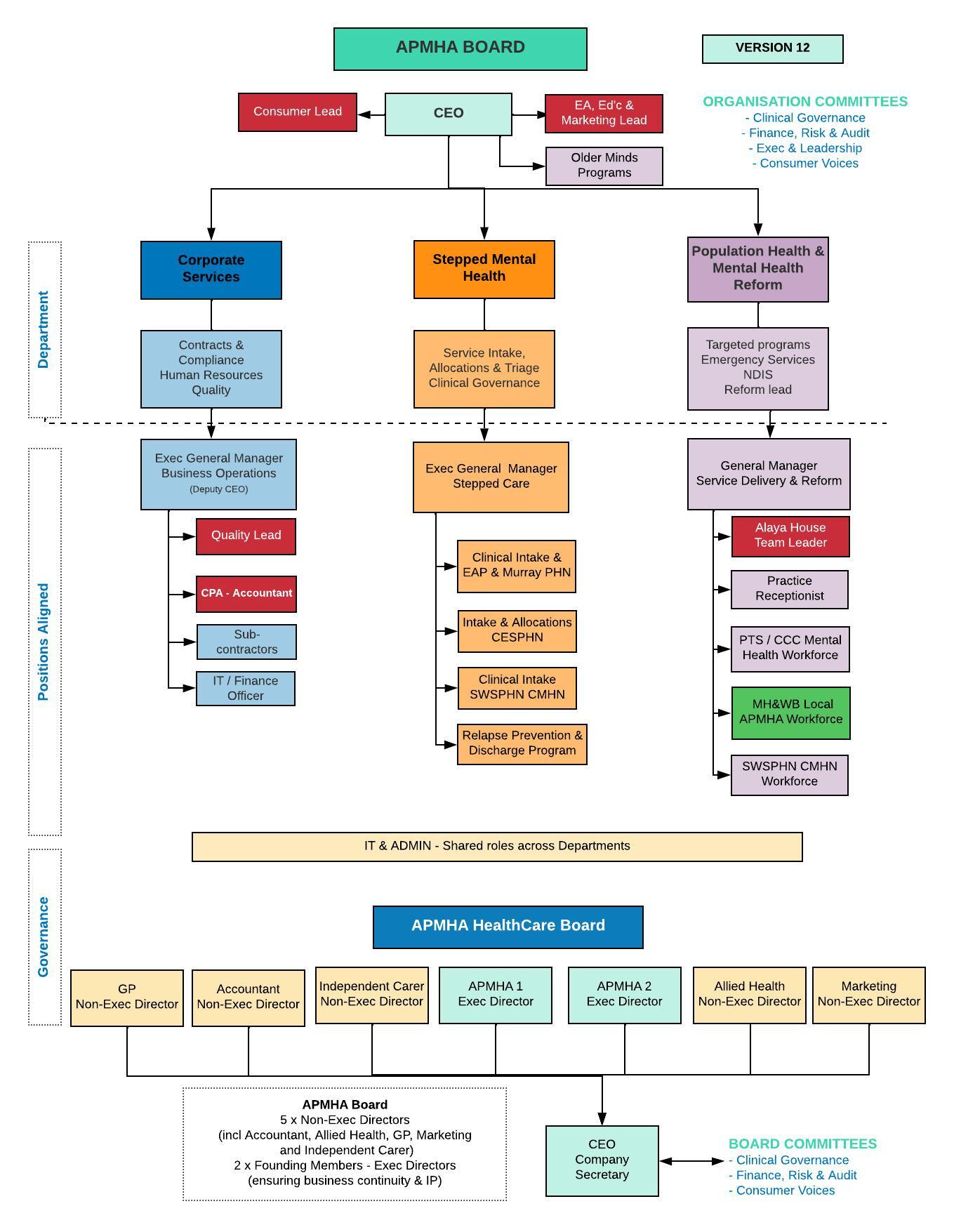
APMHA is governed by a Senior Leadership Team, an Executive Team and a Board of Management.
APMHA has two critical Board Committees which provide an avenue for input and advice by the senior leadership team into strategy and business development. These committees include:
- Clinical Governance Committee
- Finance, risk and audit Committee
APMHA HealthCare Ltd is Accredited under the following standards:
- AS/NZS ISO-9001-2016,
- National Standards for Mental Health Services – 2010
- NDIA – NDIS Registered Provider
In 2019, APMHA HealthCare realised our dream to establish our first mental health wellbeing hub located in Shepparton, Victoria. Our aim was to create a hub focused on wellness, recovery and supporting people to live a full and contributing life as determined by them. With this hub, we have created a physical presence in the region and a holistic team approach with our various funded local mental health services and workforce.
The APMHA Model of Care
APMHA offers employed, secondment and sub-contract arrangements for clinical and non-clinical workforce it engages to ensure a national footprint of highly qualified mental health professionals. APMHA has developed a Service Delivery Framework to reflect a Stepped Mental Health Model of care which sets out the strategic direction of the company, the funding it has been awarded and the partnerships it has forged.
Our Vision
An accessible primary mental health service working in collaboration to support people with a mental illness to reclaim wellbeing and live a contributing life. We will achieve our Vision through a commitment to embrace and live our Values.
We Value
- Lived Experience
- Collaborative Leadership
- Community
- Integrity
- Respect
- Innovation through passion
Our Organisation
Relapse Prevention and Discharge Program
APMHA is pleased to introduce our new pilot program – “Relapse Prevention and Discharge Program” (RP&D). This program was created in collaboration with APMHA clinicians and our Consumer Lead. The RP&D program aims to support each client before and after discharge from our programs.
The program is currently being trialed in the Goulburn Valley & North East Vic regions of Murray PHN through our primary mental health funded programs. After evaluation and any refinement, our aim is to roll this out across all APMHA services in 2025.
The RP&D pilot program has been developed to support people:
- Who have exited our programs early, providing active follow up for people who have not engaged as planned, to address any barriers they have experienced or identify any further support they may need
- Who are currently receiving mental health services by incorporating the Wellness and Discharge Planning Toolkit into counseling consultations, to ensure a wellness approach as part of therapy and support preparation for discharge from the service. This also includes post discharge follow up by our RP&D support worker.
Benefits of the Program
The program has been designed to help clients to:
- identify goals
- stay on track
- identify stressors and triggers in life
- develop positive coping strategies
- create a support network
- identify early warning symptoms
- understand medications
- feel empowered in care and post discharge goals
- know when and how to access further support when needed
- live your best life
GSSM Mental Health and Wellbeing Local
Mental Health and Wellbeing Locals provide treatment, care and support for people aged 26 years and over.

The Locals are free, voluntary and easy to access, with no referral or Medicare card required. Care will be provided for people who need more support than a general practitioner (GP) or private mental health practitioner can offer, but who do not need higher-intensity services, such as hospital-based support services.
Mental Health and Wellbeing Locals offer one-on-one support, group support and advice through listening and helping you explore the services and support right for you and your situation. Support is confidential and we will work with you to find the help you need. Mental Health and Wellbeing Locals offer:
- Treatment and therapies
- Person-centered wellbeing supports
- Education, peer support and self-help
- Care planning and coordination with various service providers
- Person-centered wellbeing supports including
- Peer Worker Education, peer support and self-help
- Participant-led care planning and coordination with other service providers
- Additional Mental health supports and resources
Mental Health and Wellbeing Locals are respectful of, and responsive to, cultural needs and diversity. All visitors will receive fair access and culturally safe and responsive services that are free of stigma and discrimination.
Location
Shepparton, Strathbogie, Moira
Phone: 1300 000 559
151-155 Maude Street, Shepparton VIC 3630
Eligibility
Anyone aged 26 years of age or older who is experiencing psychological distress, mental health challenges or alcohol and other drug concerns.
NWMPHN Older Minds Program
The service is for residents who are experiencing (or at risk of) mild to moderate mental health concerns.
This may include residents who:
- require support to adjust to life in residential aged care
- experience grief, depression, anxiety, phobia or other mild to moderate conditions
- live with pre-existing mental health conditions that do not require ongoing or intensive support through psychogeriatric services.
This service also provides mental health training for aged care facility staff to enable timely identification of psychological distress in residents and appropriate referral.
Areas of service
The local government areas for Western region include: Brimbank, Hobsons Bay, Melton, Maribyrnong, Moonee Valley, Wyndham, and Moorabool (Bacchus Marsh part).
Eligibility
Residents of registered Residential Aged Care Facilities within catchment area listed above.
Our APMHA Older Minds clinicians work collaboratively with each Facility to identify residents who may benefit from this service and will support the referral and registration process each time they visit.
6 Months in Review: Feedback from Residential Aged Care Managers
The Mental Health Provider has a structured and collaborative approach to providing care for the residents. When they visit the residence, they come and see me, communicate with me and discuss what they are going to do the day with the residents, then they visit the residents, then come back and discuss the improvements with the GP and me and informs us the plan until the next visit. Very effective.
Communication with the Counsellor. She is very approachable and is always ready to help.
Residents were provided a venue to express their inner feeling and thoughts about their life in an RACF.
The Mental Health Provider has been a wonderful asset and contribution to our residents. They communicate exceptionally well with management and the residents mental health has much improved with her visitations.
Improving the mental health of our residents Additional engagement with the residents Womens group developed improving bonds Increased emotional support Supportive approach to our staff Excellent advocacy support for our residents with other allied health
The Mental Health Provider is so passionate about caring for their patients and going above and beyond to make them comfortable. Our clinical team is extremely thankful for the excellent service they have been providing us.
Nurse Practitioner
79 Individual clients have been seen through our NP Wellbeing service receiving 268 NP service sessions.
APMHA’s Nurse Practitioner – Sian Pritchard, came on board APMHA 1st July last year to support a gap the company had identified for people requiring the skills of a Nurse Practitioner.
“As a Nurse Practitioner with specialty areas of mental health and addiction in primary care and as a credentialed mental health nurse I have a broad scope of practice. I bring a unique set of skills to the team which enhances the service delivery we can offer. In supporting other clinicians within the teams and external personnel such as GPs and specialists we can offer a level of care and treatment that can enhance people’s overall physical and emotional wellbeing assisting them to live rewarding lives. I work across two locations Geelong which I was very familiar with before coming on board and Shepparton, a new community for me which has been a lovely location to develop new relationships.
The extensions on practice that I bring as a Nurse Practitioner include being able to prescribe and /or deprescribe medications, make recommendations to other prescribing professionals about specialist medication and treatment, provide diagnostic assessments, referral to specialists and order and interpret pathology and radiology where required to ensure someone’s physical health is being considered alongside their mental health presentations. We are aware that statistically people who live with mental illness and /or addictions often develop physical health concerns that can impact their lives greatly. Being able to offer specialist mental health and addiction treatments within primary care can be incredibly supportive for GPs whose area of expertise may not be this area and whose time we know can be very limited. Working together as a team in the community, coordinating healthcare and bridging the gaps between primary care and acute care services can ensure no one falls through the gaps in our healthcare system. Well done to APMHA for understanding what the role of a Nurse Practitioner can bring to the team.
The last year has been busy but very rewarding and I am looking forward to my ongoing work in the team in supporting the health of our communities.”
Professional Development through APMHA
APMHA understands the importance of continued professional development for all staff who work in our services whether subcontracted or employed.
Due to this, APMHA funds a number of courses each year for our clinical workforce, while also providing tailored training for staff wanting to further their professional skills. This year we focused on the following courses for our clinical workforce:
Trauma Informed Care
This course focused on the foundations of Trauma Informed Care, allowing clinicians to define different types of trauma, how trauma affects people and the community and how to work effectively with clients and their trauma. This session also includes a section on trauma and its impact on the workforce.
Some feedback from this course:
- The presentation was informative, interactive and engaging. I was able to further expand my knowledge in trauma informed care and learn new skills.
- Great trauma informed information, which was presented well regarding the complexity of the topic. Easily understood information which I can work to support my own clients to understand.
- It was great to know that the clinical interventions discussed are what I am already doing with clients. Helped to reinforce my knowledge.
- I will be able to effectively support clients with the skills and knowledge I have gained from the training, I will be able to apply this learning to better understand the lived experiences of clients.
- Great training which was helpful and specific to what a lot of APMHA’s clients are experiencing. Being able to step into further understand ways to support people acknowledging what they are experiencing through collaboration, building trust/rapport was a highlight to improving our service.
Bio-Psycho-Social Training
This training focused on reviewing key concepts when undertaking the Bio-Psycho-Social Assessment and Mental State Examinations with clients. This course also looked at how information gathered from these assessments link in with the treating clinicians formulations and interventions.
Some feedback from this course:
- I really appreciated the opportunity to participate in this training – Thank You.
- I will incorporate elements of the biopsychosocial model into my initial assessment to gather further information about a client to best support their needs.
- Reenforcing my current assessments, intake and ability to gather information to ensure it is more accurate and person centred.
- This will be used all the time in my work with clients, and initial assessments with clients.
Advanced Suicide Prevention Training
This training aims to increase health professionals’ skill and confidence in taking a detailed suicide history and developing a collaborative management plan to increase the safety of people planning suicide. This course also provides practical tools for managing suicide risk presentations.
Some feedback from this course:
- I have my scripted questions now for asking about suicide. I think it will be much more likely I’ll get a response from people if they are thinking about suicide.
- I will be able to implement this knowledge in the risk assessments I conduct with clients and supporting client’s in connecting with mental health services
- A different take on suicide prevention. Practicing scenarios. Approachable presenters also working in the field like me, so knew where/how to pitch it.
- Applying the learning with clients to ensure the risk assessment completed is in accordance to what is expected and ensuring the safety of the clients.
Cultural Safety Series for Health Practitioners
This course introduces participants to some of the elements that contribute to cultural safety when working with Aboriginal and Torres Strait Islander Peoples and communities, specifically in the health and social service space. The course aims to provide targeted and practical information for health professionals.
Some feedback from this course:
- Very very useful. Provided more awareness on this topic and further knowledge building.
- Learned so much, brilliant. Ive done quite a lot of other training in this space, this was useful specific info.
- The training was wonderful and very thought-provoking
This year we had a number of employees who went through additional training to support their professional development:
Monique Ataryniw – Diploma of Quality Auditing
Being one of the first employees of APMHA, I have been fortunate enough to receive a variety of training throughout the years, depending on my role in the organisation. While I have enjoyed all training and mentoring provided to me, I have been most appreciative of the training APMHA provided to me this year, allowing me to not only complete a Diploma in Quality Auditing, but also training in Environmental Management Systems, Workplace Health and Safety Management Systems and Quality Auditing Management Systems.This training has not only allowed me to expand on my current role and understanding, but has also reinforced my chosen career path – This is why it is so fantastic to be apart of APMHA because not only do they want to help you professionally develop in your employed role, but they are also genuinely interested in supporting you develop your career pathway and professional interests.
Lauren Millar – Mental Health First Aid and Practice Receptionist Course
I’ve found the training extremely thorough and has been very beneficial for my position as Practise Receptionist. I’ve made sure to designate time to fulfill my studies, both outside of work, and when I am in office once I have ensured any work tasks are completed. I’m very appreciative to APMHA for having covered the fees associated with the course and definitely believe it is worth the time and energy put in to complete each unit.
Paul Darley – Acceptance and Commitment Therapy
ACT was an intensive 2 day course which focused on true collaboration with our clients to gain the best outcomes for them. Learning techniques about diffusion and addressing negative thoughts will be very useful and easy to utilise in practice. I feel this training aligned well with a lot of other amazing training such as motivational interviewing and collaborative recovery model but took it to a new level of actual therapeutic practice using specific strategies.
Donna Taggart – Acceptance and Commitment Therapy
Early in October 2023, I was part of a team that went to Melbourne to undertake the introductory training for Acceptance Commitment Therapy (ACT) with Russ Harris. This is a Values based modality that aligns concurrently within the PTS that we provide our clients at APMHA. Some of the new techniques I learned within that 2 day workshop include “Dropping Anchor” and “Choice Point – Towards/Away moves.” We then presented our new knowledge to the whole APMHA team in a powerpoint presentation. I was so impressed with this modality, that I have since purchased a few ACT books and resources, and more workshops and I regularly use these techniques now. It was a lot of fun and I feel very grateful. I am now a Registered ACT Therapist.

